Understanding the Interplay Between 2-OH, 4-OH, 16-OH, and 8-OH
EndoAxis Clinical Team
By now, you are likely familiar with the estrogen metabolites: 2-OH, 4-OH, 16-OH estrone/estradiol. However, did you know that the relationship between these metabolites, along with a comparison of an Organic Acid called 8-hydroxy-2′-deoxyguanosine (or 8-OHdG for short), together can give a metabolic “snapshot” of how your body is processing estrogens and how much oxidative stress may be affecting DNA and cellular health! Estrogen metabolism follows multiple hydroxylation routes. Remember that hydroxylation is the first step in detoxification for our Phase I metabolites. This process begins with the cytochrome P450s (the CYP enzymes) adding a hydroxyl group (-OH) to estrone or estradiol. Once these hydroxyl groups are added, it sets the stage for further detoxification and deactivation of these estrogens.
The hydroxylation pathways are as follows:
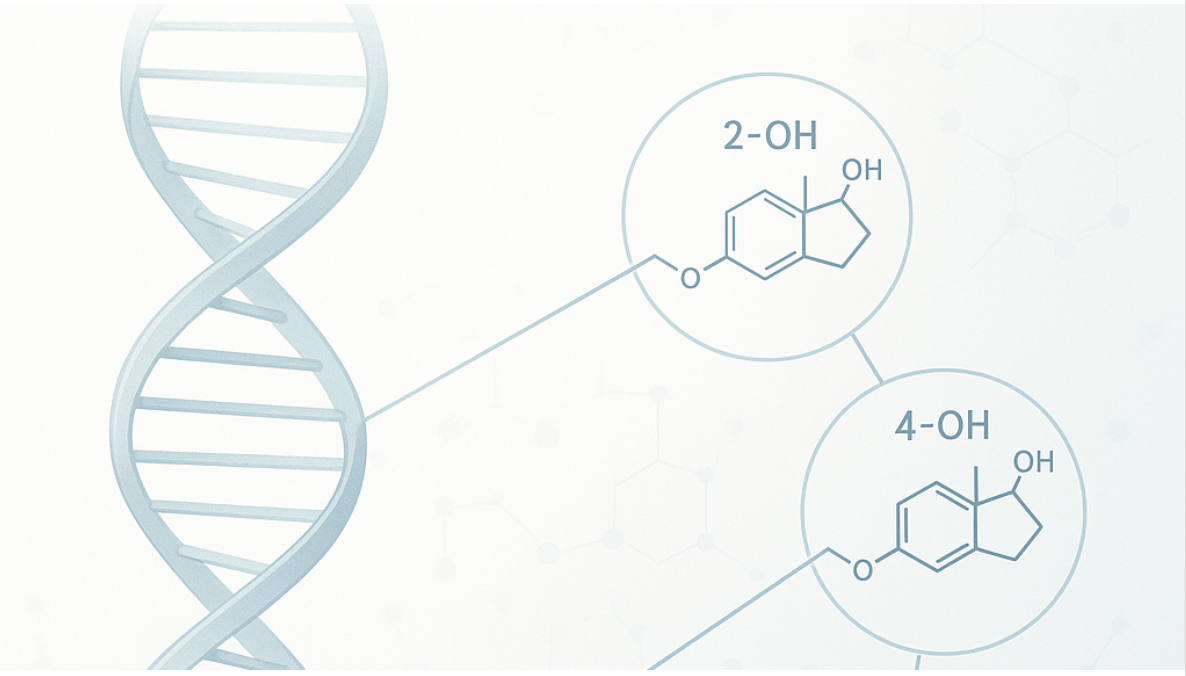
CYP1A1 → 2-hydroxyestrone/estradiol (2-OH) Generally viewed as less proliferative and often termed “protective.” We prefer to use the term “preferred” estrogen, as this 2-OH metabolite is the most stable through hydroxylation and most readily methylated. However, a common misunderstanding is that 2OH is not problematic, but remember, it is still a catechol estrogen.
CYP1B1 → 4-hydroxyestrone/estradiol (4-OH) A catechol that readily oxidizes to quinones capable of forming depurinating DNA adducts, contributing to mutagenic (cancer) risk.
*Catechol estrogens can become quinones, which damage DNA if not metabolized appropriately.
CYP3A4 → 16α-hydroxyestrone (16α-OH)A powerhouse detox pathway that so happens to also metabolize estrone to 16-OH E1, and estradiol to 16-OH E2 (also known as “Estriol”). These are NOT catechol estrogens.
16α-hydroxyestrone (16α-OH) – a proliferative metabolite that covalently binds the estrogen receptor, promoting sustained signaling and tissue growth.
Phase II Detoxification: Methylation, Glucuronidation, Sulfation
Catechol estrogen metabolites (2-OH and 4-OH) are further neutralized via COMT (catechol-O-methyltransferase) to 2-methoxy- and 4-methoxy-estrogens, reducing their reactivity.
16-OH metabolites are not methylated but undergo sulfation.
Glutathione conjugation, glucuronidation, and sulfation also help eliminate secondary metabolites and quinones.
If methylation or conjugation is sluggish (due to nutrient deficiencies, genetic variants, or oxidative stress), catechol estrogens—primarily 4-OH—can form quinones that bind DNA, leading to mutations and oxidative stress.
Catechol Estrogens Become Riskier When:
- Methylation clearance is poor
- Glutathione activity is poor (low or high pyroglutamate)
- NQO1 (NADPH-quinone oxidoreductase) is suboptimal
- NRF2 activity is poor
- NFkB activity is high (due to cytokines, ROS, heavy metals, LPS, obesity, alcohol, insulin resistance, stress, etc.)
When NFkB is high, NRF2 and glutathione are suppressed, increasing intracellular free radical activity.
The Ratio Perspective
A high 2-OH / 16α-OH ratio is generally favorable (more detoxification, less proliferation).
A high 4-OH fraction indicates potential oxidative risk if not balanced by methylation or antioxidants.
This pattern is often assessed in DUTCH or urinary estrogen metabolite panels.
Adding To The Detox Picture: 8-OHdG
8-Hydroxy-2′-deoxyguanosine (8-OHdG) is a urinary or serum marker of oxidative DNA damage that reflects oxidative stress at the DNA level.
Elevated 8-OHdG suggests oxidative stress is outpacing antioxidant protection due to:
- Low glutathione or antioxidant capacity
- Inflammation
- Poor mitochondrial efficiency
- Excess estrogen quinone formation
Why This Combination Matters
The oxidative metabolism of estrogens doesn’t occur in isolation.
Reactive oxygen species (ROS) generated during catechol oxidation amplify DNA damage, while proliferative signaling from 16α-OH increases mutational risk.
Together, these pathways connect metabolic activity with oncogenic potential.
Clinical Pearl
Epidemiology: The “2:16 ratio” once used as a breast cancer risk marker is inconsistent in large studies. However, 4-OH metabolism, quinone adducts, and DNA damage remain strongly linked mechanistically.
Lifestyle Impact: Smoking, obesity, inflammation, alcohol, and endocrine disruptors upregulate CYP1B1 and increase quinone formation.
8-OHdG Context: Reflects total body oxidative stress, not estrogen-specific, but reinforces metabolic-genotoxic overlap when paired with estrogen metabolite imbalances.


