EndoAxis Clinical Team

Hormonal contraceptives are widely used for birth control and symptom management, but they introduce complex challenges when it comes to interpreting sex hormone panels. For clinicians evaluating patients on hormonal birth control, understanding the pharmacological intent and physiological impact of these medications is critical to determine whether hormone testing is clinically meaningful—or potentially misleading.
Understanding Hormonal Birth Control’s Impact on Endogenous Hormone Production
Hormonal birth control—including oral contraceptive pills (OCPs), progestin-only pills, implants (e.g., Implanon), and injections (Depo-Provera)—exert their contraceptive effects primarily by suppressing the hypothalamic-pituitary-ovarian (HPO) axis.
By delivering synthetic forms of estrogen, progestin, or both, these medications:
- Prevent ovulation
- Thicken cervical mucus
- Alter the endometrium
A critical consequence of this suppression is the downregulation—or functional “shut-off”—of endogenous hormone production from the ovaries.
In this context, testing sex hormones is often considered an ineffective use of resources. Treatment aimed at “balancing” hormones that are pharmacologically suppressed is functionally irrelevant, as the root physiology is being pharmacologically overridden. Recommendations based on these results often “fall on deaf ears” within the body—unable to influence a system that is under the dominant control of a strong synthetic agent.
Nutrient Depletion from Hormonal Contraceptives
One of the most clinically relevant interventions for women on hormonal birth control is nutrient repletion. These medications are known to deplete or interfere with the absorption, synthesis, or metabolism of multiple key nutrients:
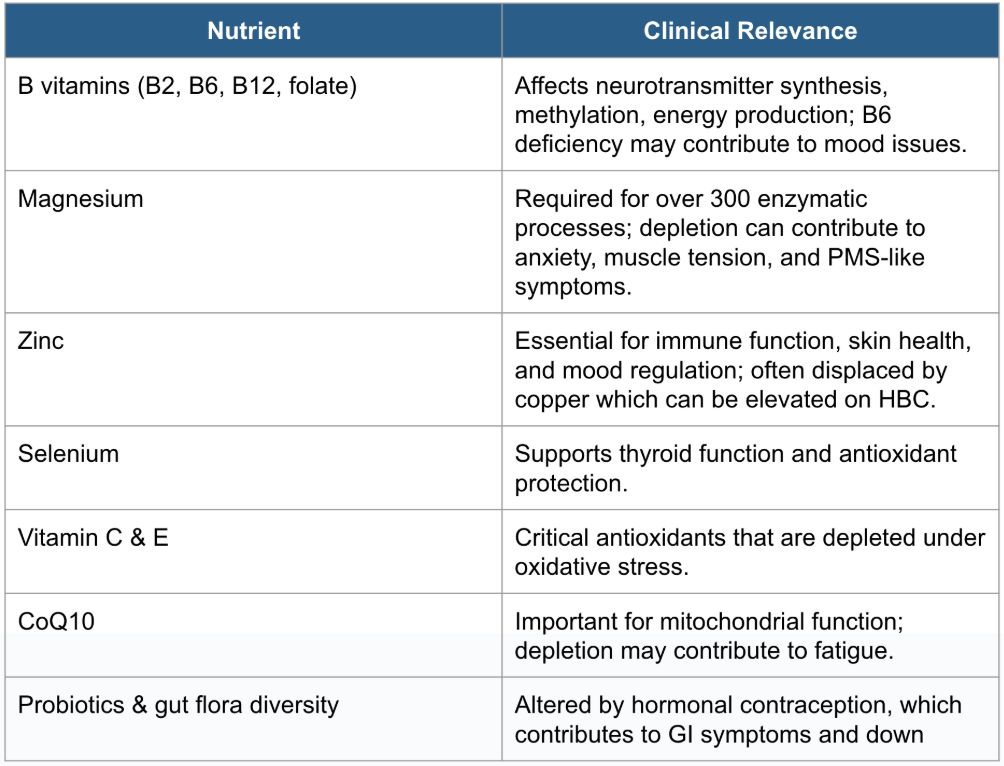
Repletion of these nutrients—ideally through a combination of diet and supplementation—can be a foundational and impactful intervention to optimize resilience and counteract side effects from hormonal birth control.
Liver and Gut Stress from Synthetic Hormones
Given the intended pharmacological suppression of the HPO axis, testing for endogenous sex hormones while a patient is on systemic hormonal contraception is generally not recommended.
- Test results reflect an artificially altered endocrine environment.
- Results cannot be used to make accurate inferences about underlying hormonal imbalances or physiologic function.
- Exogenous synthetic hormones (e.g., ethinyl estradiol, levonorgestrel, medroxyprogesterone) are not detectable on standard sex hormone assays, so the full hormonal landscape cannot be accurately assessed.
Attempting to “correct” hormone patterns while a patient remains on hormonal contraception is also problematic:
Without the ability to adjust endogenous hormone production—which is pharmacologically suppressed—intervention becomes both ineffective and potentially harmful.
Adding bioidentical hormones or supplements aimed at modifying estrogen or progesterone levels can disrupt the already medicated hormonal feedback loops.
This can stress hepatic clearance pathways and worsen symptom burden.
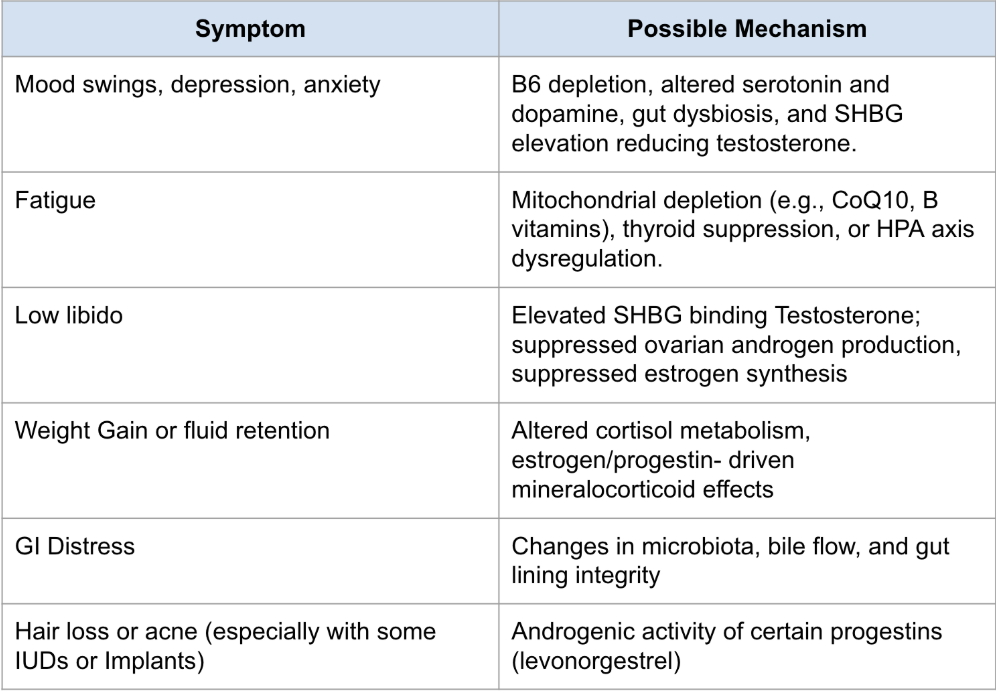
Common Symptoms While on Hormonal Birth Control
Despite being used to “manage” symptoms like acne, painful periods, or irregular cycles, many patients develop new or persistent symptoms while on hormonal contraception:
Supportive Clinical Approach
Step 1: Restore nutrients with a high-quality multivitamin, targeted B vitamins, magnesium, zinc, and antioxidants.
Step 2: Support adrenals & thyroid with appropriate lab testing and individualized care.
Step 3: Repair gut health with probiotics, antimicrobial herbs, and dietary changes. Herbal hormone balancing or bioidentical hormones generally do not work while on systemic contraception, since ovulation and normal hormone cycling are suppressed.
When Symptoms Persist
If the patient remains symptomatic despite comprehensive nutrient and organ system support, it becomes appropriate to have a values-based discussion around the role of hormonal birth control as a potential “obstacle to cure.”
Key considerations for this conversation include:
- Patient goals: Are they seeking long-term symptom resolution or symptom management?
- Reproductive planning: Is birth control needed for contraception or symptom suppression?
- Autonomy and education: Does the patient understand how hormonal contraception may be perpetuating or exacerbating their symptoms?
For some, transitioning off hormonal birth control and toward a fertility awareness method or non-hormonal option may allow for more direct assessment and treatment of underlying hormone imbalances.
For others, remaining on hormonal contraception with supportive therapies may be the best short-term solution, with regular reassessment.
Summary
Women on hormonal birth control deserve a nuanced, respectful, and physiology-based approach to care. Testing endogenous sex hormones while on hormonal contraception rarely yields actionable insights and can mislead treatment planning. Remember that trying to alter or replace hormone activity directly while on a suppressive therapy like hormonal birth control is at odds with the mechanism of action of the hormonal contraceptive and can lead to erratic physiology and a worsening of symptoms. Instead, focus on nutrient restoration, biliary and gut support, adrenal and thyroid testing, and symptom-driven care. When symptoms persist despite these interventions, the hormonal contraceptive itself may need to be reconsidered in the context of the patient’s long-term goals and whole-person health.


