Considerations for Supplements, Medications, and Timing
EndoAxis Clinical Team

Although we have talked a lot about urinary hormone testing and considerations, serum testing is equally important in identifying key aspects of hormone balance and in diagnosis and management of many hormone-related conditions. Serum hormone testing is a cornerstone of managing patients on bioidentical hormone replacement therapy (BHRT) and other endocrine interventions. Yet, multiple factors—from supplements to medications and the timing of dosing—can significantly influence lab results, potentially leading to misdiagnoses or inappropriate treatment adjustments.
High-Dose Biotin: A Common but Underrecognized Lab Interference
Biotin, often marketed for hair, skin, and nail support, is one of the most frequent causes of lab interference.
In fact, on Nov. 28, 2017, the FDA issued a safety communication indicating that biotin in specimens from people taking biotin supplements may cause interference with some laboratory assays. The warning stated, “The FDA is alerting the public, health care providers, lab personnel, and lab test developers that biotin can significantly interfere with certain lab tests and cause incorrect test results, which may go undetected.”
High circulating biotin from supplementation can interfere with a variety of diagnostic tests, including:
- Thyroid function tests: Causes falsely low TSH values and falsely high free T3, free T4, total T3 and total T4 values. This can mask hypothyroid concerns and may incorrectly appear like hyper-thyroid disease. This is why labs like Quest and LabCorp stipulate avoidance of biotin for at least 72 hours before testing thyroid labs.
- Troponin assays: Results in falsely low troponin levels, which could lead to doctors missing a critical elevation in a marker that indicates heart attack diagnoses
- Infectious disease markers: including falsely low hepatitis and COVID-19 assays
- Hormone labs: May falsely elevate estradiol and progesterone, while potentially causing a falsely low insulin level, LH, FSH, prolactin and PSA lab value.
Mechanism: The lab error is specific to immunoassay-based labs. The reason for the lab error is because immunoassays rely on biotin-streptavidin binding to detect specific proteins. Excess biotin in the blood competes with reagents, producing falsely elevated or depressed results depending on the assay.
Clinical note: Advise patients to discontinue biotin-containing supplements at least 72 hours prior to lab testing. Always review supplement lists when unexpected lab results arise.
Other Supplements and Medications That Can Affect Labs
Supplements
- Vitamin C: May elevate blood glucose readings. Vitamin C may also lead to false-negative results on some fecal occult blood tests (screening tools for colorectal cancer).
- Calcium: Can falsely influence bone density results if taken on the same day as their DEXA scan.
- Creatine: Can elevate serum creatinine, mimicking kidney dysfunction.
- Order a Cystatin C if a patient is on creatine, and kidney health is a concern. Cystatin C is a more accurate measure of kidney function, and will not be impacted by supplements.
Medications
- Thyroid medications (levothyroxine): Optimal absorption requires fasting; timing affects TSH and free T4 results.
- Thyroid medication should not be taken the morning of a thyroid lab.
- Patients should be instructed to take their thyroid medication the day before, but NOT the morning of the blood test. After their blood draw, they can take their morning thyroid dose.
- Corticosteroids: Can suppress endogenous cortisol production, affecting adrenal function tests. Avoid testing cortisol activity if a patient was recently on a glucocorticoid.
- Anticonvulsants: Alter estrogen metabolism, potentially affecting sex hormone panels. Knowledge is key – as avoidance of this medication may not be possible. If you know how a medication will alter blood work, you can account for abnormalities that may arise.
Clinical Takeaway
A comprehensive review of both prescription medications and over-the-counter supplements is essential for accurate lab interpretation.
Timing Matters: Hormone Testing and Dosing Considerations
The timing of hormone testing relative to dosing is critical, particularly in BHRT:
Testosterone: Levels fluctuate diurnally. Morning testing, when endogenous levels peak, provides the most accurate snapshot.
Estrogen and Progesterone: For menstruating women, testing should align with specific cycle days (e.g., LH and FSH to measure baseline levels on cycle day 3 (or roughly days 2-5); progesterone and estrogen can be collected on days 19–22, when progesterone would peak if ovulation occurred).
Postmenopausal women can test at random, but should aim for a morning blood draw, and should collect their labs at roughly the same time every time they check their values (e.g., if they get their blood tested at 9am, they should always test around 9am for any future hormone panel).
Medication coordination: Align serum lab draws with hormone dosing schedules to avoid transient spikes or troughs that may misrepresent steady-state levels.
- Oral and sublingual medications:
- Estradiol, Testosterone and DHEA: Draw blood at least 24 hours after the last dose of bHRT to review their steady-state levels in serum.
- Progesterone: Due to a very short half-life, progesterone can be taken the night before a morning blood draw.
- Topical creams, gels and patches: the washout period is often 48–72 hours, since absorption is variable and peaks can be prolonged.
- Stop all topical hormones at least 48 hours prior to a morning blood draw to review their steady-state levels in serum.
- Pellets and injections: testing should be standardized to a fixed time after the last administration. Generally, half-way between pellet reinsertion or injection will reveal the steady-state hormone levels in serum.
Clinical pearl: Notice how the duration of avoidance for oral/sublingual vs topical applications are opposite in serum vs urinary testing. This is due to the absorption and pharmacokinetics of the medications as they relate to circulation and elimination.
Best Practices for Accurate Hormone Testing
1. Pre-Test Preparation: Fasting as indicated; discontinue interfering supplements (biotin, high-dose vitamin C, etc.) for 48–72 hours.
2. Consistent Timing: Test at the same time of day, ideally morning, to account for diurnal hormone fluctuations.
3. Medication Coordination: Consider last dose timing for BHRT and other hormone-modulating medications.
4. Comprehensive Review: Assess all prescription, over-the-counter medications, and supplements for potential assay interference.
5. Patient Education: Emphasize adherence to pre-test instructions for reliable results. By carefully considering supplement use, medication timing, and dosing schedules, clinicians can optimize the accuracy of hormone testing. This reduces the risk of misinterpretation, allows for precise clinical decision-making, and ensures that patients receive the most effective, individualized care.
Quick Reference Overview
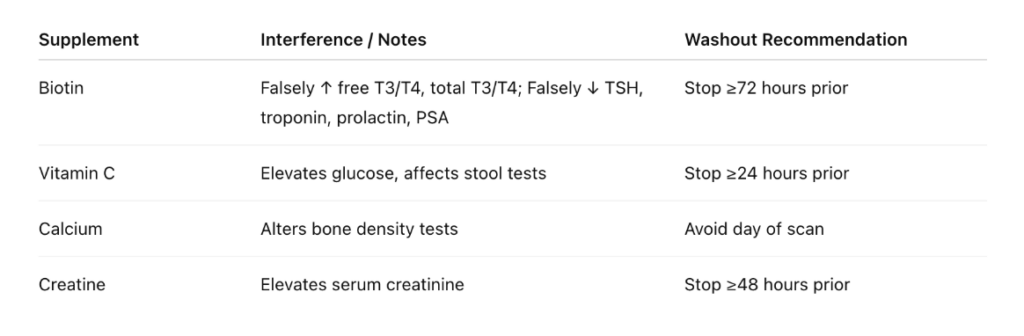
Additional Tips
- Maintain consistent timing
- Consider route of administration
- Factor in fasting, exercise, circadian rhythm
Key Clinical Takeaways
- Review all meds/supplements before testing
- Educate patients on washouts
- Coordinate with BHRT dosing + menstrual cycle
- Watch for unexpected results that may indicate assay interference


