EndoAxis Clinical Team
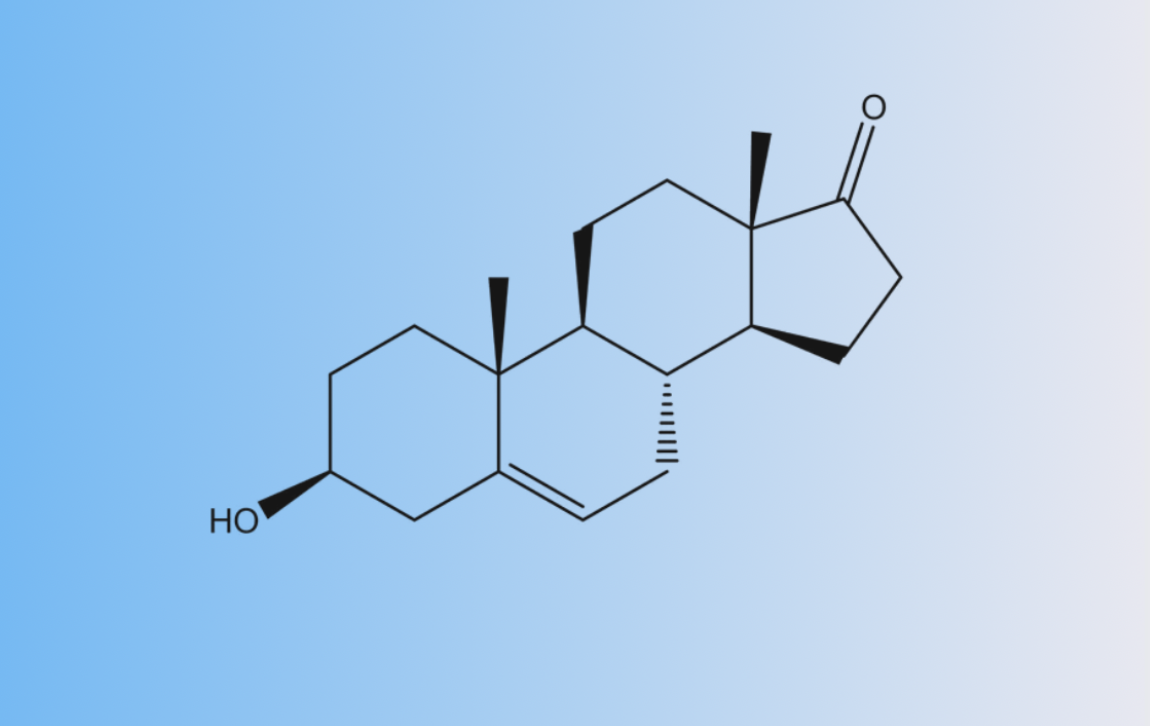
DHEA (Dehydroepiandrosterone)
- The parent hormone made by the adrenal glands (and to some extent the gonads).
- Short half-life (~15–30 minutes).
- Highly dynamic, fluctuates throughout the day from its diurnal pattern.
- Can convert into DHEA-S, testosterone, estrogens, and other androgens.
- Bioactive, but mostly a precursor or “reservoir” in hormone pathways.
DHEA-S (Dehydroepiandrosterone sulfate)
- Sulfated, more stable version of DHEA.
- Much longer half-life (~7–10 hours).
- Does not easily convert back into DHEA but reflects overall adrenal androgen output.
- ~98% of DHEA in the body exists as DHEA-S.
- Not as bioactive, more of a storage form or indicator of supply line health.
Enzymatic Regulation
SULT2A1 (Sulfotransferase 2A1)
- Catalyzes DHEA → DHEA-S (sulfation)
- Predominantly active in the liver and adrenal cortex
- Activity is:
- Downregulated by inflammation, LPS (gut-derived endotoxin) → increases downstream androgen/estrogen metabolism
- Upregulated by glucocorticoids (e.g., dexamethasone) and spironolactone → favors DHEA-S storage
STS (Steroid Sulfatase)
- Catalyzes DHEA-S → DHEA (desulfation), reactivating it for conversion to sex hormones
- Highly active in adipose tissue, skin, prostate, endometrium, and placenta
- Activity is:
- Inhibited by medications (e.g., bupropion, benzodiazepines, alcohol) → elevated DHEA-S
- Upregulated in estrogen-dominant states, genetic polymorphisms, and potentially by certain flavonoids (e.g., quercetin) → lowers DHEA-S
Serum vs Urine Testing: How Do Levels Compare?
Serum (Blood) Testing
- DHEA-S is best tested in serum due to stability and standard reference ranges.
- DHEA can be tested in serum, but due to its short half-life and fluctuations, it’s less reliable unless doing multiple time points.
Clinical Pearls:
- Serum DHEA-S is often used as a marker of adrenal function, particularly in:
- Adrenal fatigue/insufficiency
- PCOS (often elevated)
- Age-related decline
- It’s a good “set point” measure — less influenced by acute stress or diurnal variation.
Urine Testing (DUTCH or 24-hour)
- Measures DHEA metabolites (DHEAs + Etiocholanolone + Androsterone).
- Does not directly measure DHEA
- Provides insights into how DHEA is being metabolized downstream into androgens or estrogens.
- Better at reflecting long-term hormone output and detoxification routes.
- Provides insights regarding potential inflammation, hormone imbalance or adrenal stress.
Clinical Pearls:
- Useful when you want to see enzyme activity and conversion patterns—how DHEA is pushed toward testosterone vs estrogen, for instance.
- Helpful for root cause work in androgen-dominant patterns, adrenal dysfunction, or when serum values don’t match the symptoms.
- Identifying issues with STS or SULT2A1 activity
How Does EndoAxis Help with DHEA Levels and Test Results?
EndoAxis technology analyzes urinary hormone data through a pattern-based lens, incorporating symptomatology and comprehensive steroid pathways. By integrating cortisol, DHEA, DHEA-S, and sex hormones, the platform helps clinicians:
- Identify enzyme imbalances (e.g., STS, SULT2A1 dysfunction)
- Determine when DHEA supplementation may be appropriate—or contraindicated
- Understand individual tendencies toward androgenic or estrogenic dominance
- Optimize therapeutic decisions using holistic hormone data in context
A nuanced understanding of DHEA and DHEA-S—alongside their regulating enzymes and appropriate testing methods—enables more accurate diagnosis and individualized hormone interventions. When paired with clinical context and pattern recognition tools, EndoAxis can more precisely tailor therapies for hormonal balance and improved patient outcomes.
References
Brahimaj A, Muka T, Kavousi M, Laven JS, Dehghan A, Franco OH. Serum dehydroepiandrosterone levels are associated with lower risk of type 2 diabetes: the Rotterdam Study. Diabetologia. 2017 Jan;60(1):98-106. doi: 10.1007/s00125-016-4136-8. Epub 2016 Oct 22. PMID: 27771738; PMCID: PMC6518366.
Parikh TP, Stolze B, Ozarda Y, Jonklaas J, Welsh K, Masika L, Hill M, DeCherney A, Soldin SJ. Diurnal variation of steroid hormones and their reference intervals using mass spectrometric analysis. Endocr Connect. 2018 Dec;7(12):1354-1361. doi: 10.1530/EC-18-0417. PMID: 30400040; PMCID: PMC6280590.


